Researchers from across the globe looked at the global impact of the pandemic on attitudes and uptake of teleaudiology
The overwhelming response from the audiology community to the Covid-19 pandemic in 2020 was:
What can I do for clients? … How can I continue to help them? … Will I keep my job?
A common early reaction was to consider teleaudiology. The concept had already been around for a few decades but had never really caught on.
In mid-2020, just months into the pandemic, together with some colleagues across the globe, we set out to capture the international impact of the pandemic on audiology and gauge the uptake of teleaudiology.
Impact of the pandemic on attitudes and practice
We surveyed 337 clinicians and found that the overall attitude to using teleaudiology pre-Covid-19 was ambivalent at best.
- 43% of respondents said teleaudiology was important before Covid-19.
- 35% were neutral.
However, the pandemic appeared to change this attitude.
- A whopping 86% said that teleaudiology was important post-Covid-19.
- Only 11% remained undecided.
In fact, many clinicians started using teleaudiology in their clinics, with over 60% using it during the pandemic, compared to 42% pre-Covid-19.
Many modes were used for remote consultations, but the most popular were telephone and video conferencing.
On the other hand, audiologists reported some concerns, most notably with the quality of services delivered (e.g. patient/clinician relationships, which services could be delivered by teleaudiology). They also wondered whether their clients could cope with the technologies required for these consultations.
Facilitating teleaudiology services in the future
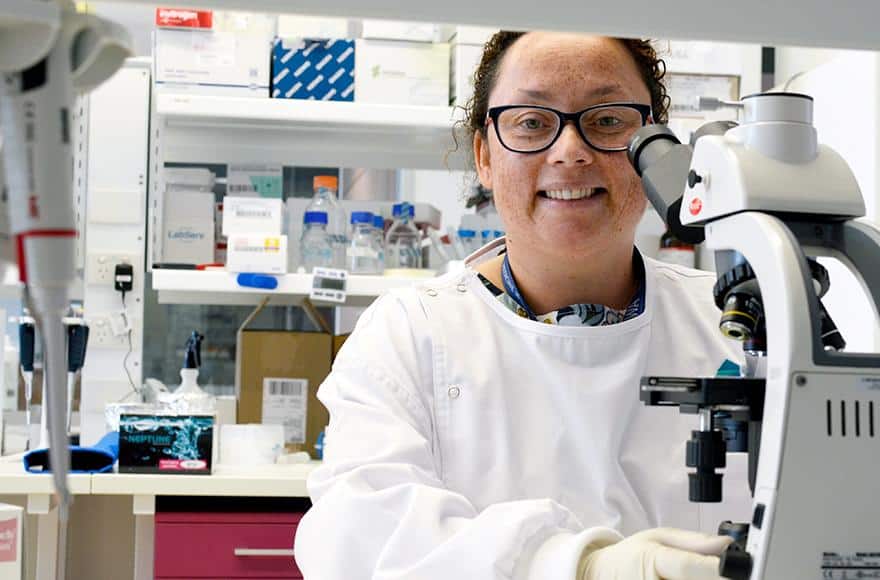
At Ear Science Institute Australia, we undertook a review to investigate the evidence supporting the safe and effective use of teleaudiology across the range of audiology services.
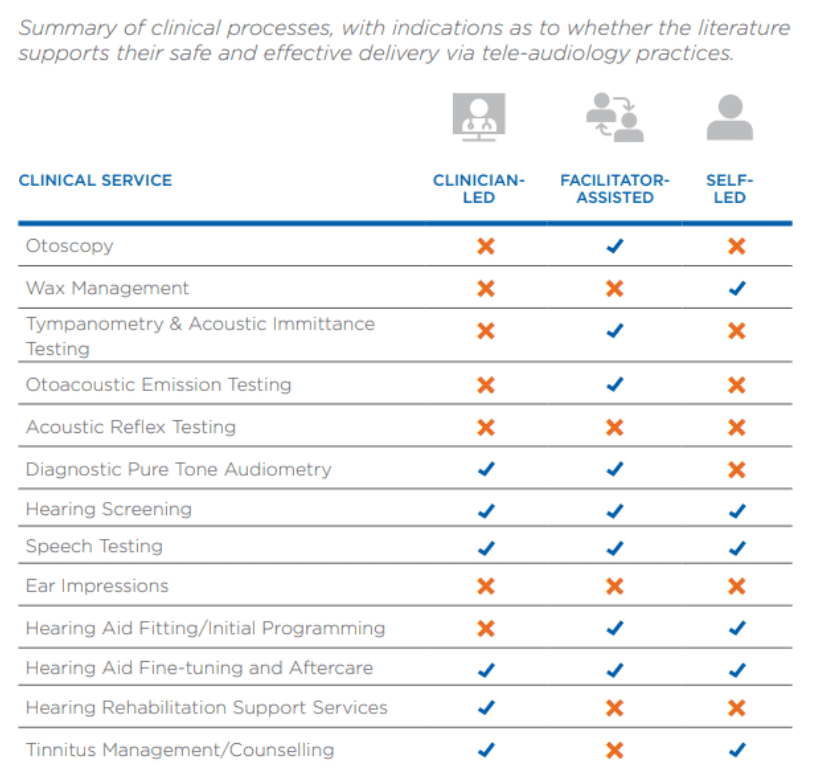
Searching published research papers, conference abstracts and reports we found evidence that supports the safe and effective use of teleaudiology for almost every clinical audiology service (See table). These services have been either clinician-led, facilitator-led, or self-led. The only services for which no evidence was found were for acoustic reflex testing and making ear impressions.
Key recommendations
- Development of clinical practice guidelines to ensure that teleaudiology services are effectively and safely delivered.
- Increase in training and infrastructure for teleaudiology.
- Raising public awareness of teleaudiology services.
- Further research, especially on the cost-utility of teleaudiology services.
Our report led to the development of the Australian Teleaudiology Guidelines. To learn more about these guidelines, I invite you to read Dr Bec Bennett’s previous blog article.
References
- Bennett RJ, Eikelboom RH, Manchaiah V, Badcock J, Swanepoel DW. International Survey of Audiologists during the COVID-19 pandemic: Effects on mental well-being of audiologists. International Journal of Audiology. 61(4):273-282; 2022.
- Eikelboom RH, Bennett RJ, Manchaiah V, Parmar B, Beukes E, Rajasingam SL, Swanepoel DW. International Survey of Audiologists during the COVID-19 pandemic: Use of and attitudes to telehealth. International Journal of Audiology. 61(4):283-292; 2022.
- Manchaiah V, Eikelboom RH, Bennett RJ, Swanepoel DW. International survey of audiologists during the COVID-19 pandemic: Effects on the workplace. International Journal of Audiology. 61(4): 265-272; 2022.
- Eikelboom RH, Bennett RJ, Brennan M. Tele-audiology: An opportunity for expansion of hearing healthcare services in Australia. Ear Science Institute Australia, Perth, Western Australia. 2021. https://www.earscience.org.au/wp-content/uploads/2021/07/TeleAudiology-Report.pdf
Republished with permission from Phonak
Derived from Phonak Audiology Blog found here | https://audiologyblog.phonakpro.com/teleaudiology–boosted-by-the-pandemic/
Published December 20, 2022.